Diabetes
Tackle Diabetes With a Plant-Based Diet
A plant-based diet is a powerful tool for preventing and managing type 2 diabetes, and even putting type 2 diabetes into remission.
The Underlying Cause of Type 2 Diabetes: Fat Accumulation Inside the Cells
Many people believe type 2 diabetes is a result of eating too much sugar, but it’s a lot more complex than that.
Insulin is a hormone secreted from the pancreas, specifically from beta cells in the pancreas, in response to rising blood sugar levels after we eat. Insulin then acts as a key to “unlock” the cells so that the glucose can move from the blood into the cells, where it can be used to produce energy. Most of the glucose gets taken up by our muscle and liver cells.1
Too much fat stored inside our muscle and liver cells, as well as elevated free fatty acids in the blood and the resultant inflammation, prevent these cells from functioning normally. For example, when there is too much fat inside our muscle cells, they are less responsive to insulin and become insulin resistant, which means they take up less glucose, leading to higher levels of glucose in the blood.1 This can be due to consuming too many calories in total, and too many calories from saturated fat. One randomized controlled trial found that after four weeks of consuming a high-fat diet (which was high in total and saturated fat) the participants’ sensitivity to insulin was reduced.2 But the good news is that a low-fat, plant-based diet can remove this excess fat from the cells and improve blood glucose control; see below for more details.
There are other compounds present in certain foods that have also been linked to an increased risk of type 2 diabetes. These include nitrates and nitrites, which are natural compounds that are commonly used to preserve meat; heme iron, which is the type of iron in meat, eggs, and dairy products; and advanced glycation end products.3-5
Preventing Type 2 Diabetes
It has been estimated that a suboptimal diet is responsible for more than 70% of new cases of type 2 diabetes.6 Vegan and vegetarian diets have been consistently found to be protective against developing type 2 diabetes. The Adventist Health Study 2, which looked at nearly 61,000 people, found that the incidence of diabetes was 2.9% in those consuming a vegan diet compared with 7.6% in nonvegetarians.7 Specific food groups have also been found to increase or decrease the risk of type 2 diabetes.
Processed meat: Aside from being classified as a carcinogen for colorectal cancer by the World Health Organization, processed meat increases the risk of type 2 diabetes more than any other type of meat.8,9 Consuming processed meat is estimated to result in one in five new cases of type 2 diabetes.6
Red meat: Weekly total meat consumption over 17 years has been associated with a 74% increased risk of developing diabetes compared with a vegetarian diet.10 Just two servings of red meat per week have been associated with an increased risk of type 2 diabetes, while replacing one serving of red meat per day with legumes or nuts is associated with a 30% reduced risk of type 2 diabetes.11
Whole grains: Whole grains are protective against type 2 diabetes.12 A comprehensive meta-analysis of prospective studies and randomized controlled trials found that compared with those who rarely or never ate whole grains, those who consumed just 48-80 grams per day had a 26% lower risk of developing type 2 diabetes.13
Fruit: A common misconception is that fruit should be avoided in people with type 2 diabetes because it is high in sugar. However, the sugar in fruit is not the same as the sugar found in refined foods. The sugar in fruit comes packaged together with fiber, phytochemicals, antioxidants, and more. Research has found that those who eat more fruit have a lower risk of developing type 2 diabetes.14-16 And in those who already have type 2 diabetes, fruit can improve blood sugar control.17,18
Sugar-sweetened beverages (SSBs): SSBs, which include drinks such as sodas, energy drinks, sweetened tea, and sweetened juices, have consistently been shown to increase the risk of type 2 diabetes. One large meta-analysis found that every serving of SSB consumed per day increased the risk of type 2 diabetes by 27%.19 SSBs can increase the risk of obesity and may lead to chronic inflammation in the body, which are two of the proposed reasons why SSBs increase the risk of type 2 diabetes.20
Managing Type 2 Diabetes
In our clinical research studies here at the Physicians Committee for Responsible Medicine, we’ve put a plant-based diet to the test with thousands of patients who have type 2 diabetes.
In 2006 we randomized 99 individuals to follow either a low-fat, plant-based diet or the American Diabetes Association’s recommended diet for 22 weeks.21 Forty-three percent of the vegan group were able to reduce their diabetes medications compared with 26% of the ADA group. And those following a vegan diet had significantly greater improvements in body weight, HbA1c, and LDL cholesterol.
A 16-week randomized controlled trial we published in 2018 found that a low-fat, plant-based diet significantly improved the function of beta cells, the pancreatic cells that secrete insulin, and insulin resistance (measured using the Homeostasis Model Assessment – HOMA-IR).22
Another 16-week randomized controlled trial we published in 2020 measured the intracellular fat found in liver and muscle cells.23 After following a low-fat, vegan diet, the mean hepatocellular fat (in liver cells) was reduced by 34.4%, and the myocellular fat (in muscle cells) was reduced by 10.4%. These reductions in intracellular fat correlated with lower insulin resistance, showing that we can reverse the underlying cause of type 2 diabetes described above.
In 2023, researchers showed that a whole food, plant-based diet can improve insulin resistance in as little as seven days.24 Individuals with type 2 diabetes who were dependent on injecting insulin were enrolled in a crossover trial comparing the Dietary Approaches to Stop Hypertension (DASH) diet and a whole food, plant-based diet. The whole food, plant-based diet was more effective than both their starting diets and the DASH diet, resulting in lower insulin doses, improved insulin sensitivity, and improved blood sugars, all within just seven days.
Mechanisms by Which a Low-Fat, Plant-Based Diet Improves Glucose Control
Weight loss: Weight loss, if a person is overweight, is a key factor for improving glycemic control. A meta-analysis published in 2017 estimated that each kilogram of weight lost is associated with a 0.1 percentage point reduction in HbA1c.25 The randomized clinical trials published by the Physicians Committee, mentioned above, have shown that weight loss is correlated with a reduced HbA1c. Weight loss resulting from a plant-based diet is often attributed to a lower caloric density of the food consumed, resulting in decreased energy intake, as well as lower fat and higher fiber intakes.
Reduced intracellular fat: Fat accumulating within muscle and liver cells causes insulin resistance, as described above. In a 2020 randomized controlled trial by the Physicians Committee, we found that reducing the fat inside these cells improves insulin sensitivity and beta cell function.23
Reduced saturated fat intake: Animal products are a major source of saturated fat in the American diet. A diet high in saturated fat has been shown to reduce insulin sensitivity in as little as four weeks in individuals with a normal insulin sensitivity at baseline, despite no changes in their body weight.2
Increased fiber: Consuming more fiber, which is exclusively found in plants, is associated with improved blood sugar control.26 This is mainly because fiber slows down the rate of absorption of glucose from the gut.
If you would like to book a consultation with a plant-based health professional to help you manage your type 2 diabetes, you can find one through our Find a Doctor network.
Plant-Powered Prescription
- Cut out animal products from your diet, starting with red and processed meats, for better blood sugar control.
- Focus on high-fiber plant foods like fruits, vegetables, legumes, and whole grains.
- Keep overall fat low in your diet by avoiding fried and oily foods.
- Minimize added sugars and sugar-sweetened beverages.
A plant-based diet is a powerful tool for preventing, managing, and even reversing type 2 diabetes. Not only is this the most delicious ‘prescription’ you can imagine, but it’s also easy to follow. Unlike other diets, there’s no calorie counting, no skimpy portions, and no carb counting. Plus, all the ‘side effects’ are good ones.
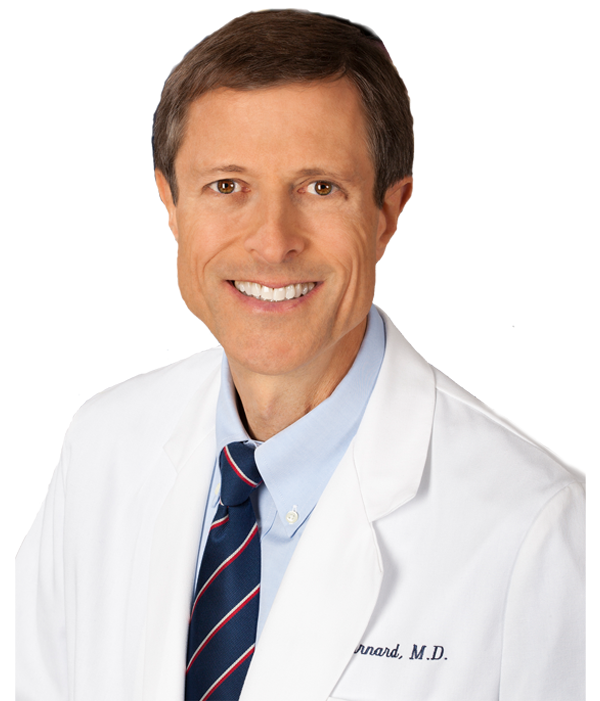
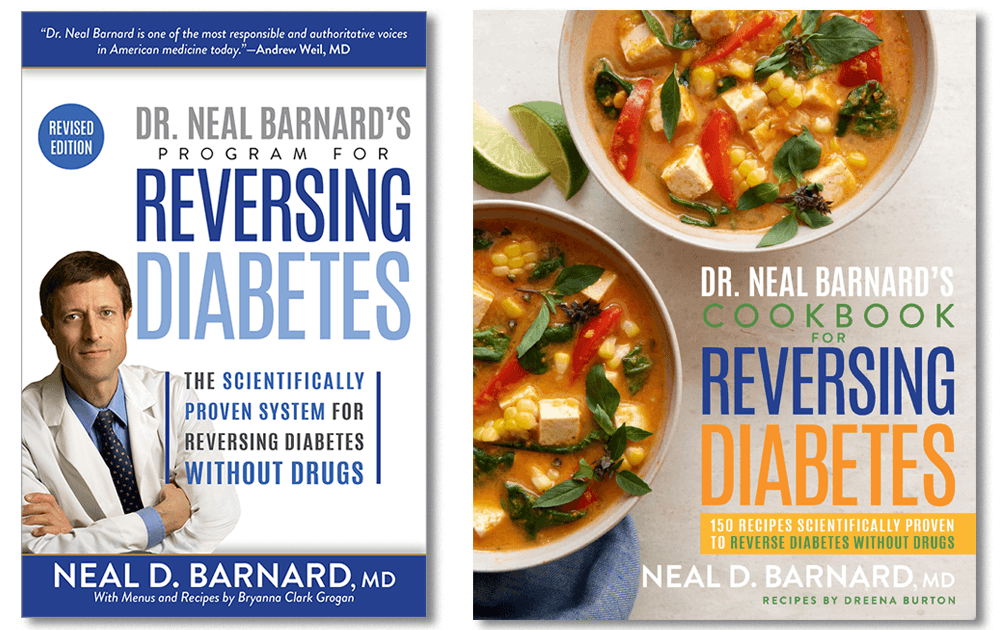
Neal Barnard, MD, FACC, President, Physicians Committee
Here’s how to tackle diabetes in a few simple steps:
Eat a plant-based diet.
Evidence shows a diet of fruits, vegetables, whole grains, and legumes can prevent and reverse diabetes.
Limit high-fat foods.
Diets high in animal products and added oils are linked to increased diabetes risk.
Eat foods that are low on the glycemic index.
Beans, oats, sweet potatoes, and other low-GI foods do not spike blood sugar.
Eat about 40 grams of fiber per day.
Found only in plants, fiber helps improve blood glucose control.
Best Foods for Diabetes
Dr. Cyrus Khambatta and Robby Barbaro are the authors of "Mastering Diabetes The Revolutionary Method to Reverse Insulin Resistance Permanently in Type 1, Type 1.5, Type 2, Prediabetes, and Gestational Diabetes"
Diet and Diabetes: Recipes for Success
To order Diet and Diabetes: Recipes for Success as a printed booklet, please visit our Physicians Committee Shop.
Diet and Diabetes: Recipes for Success in other languages
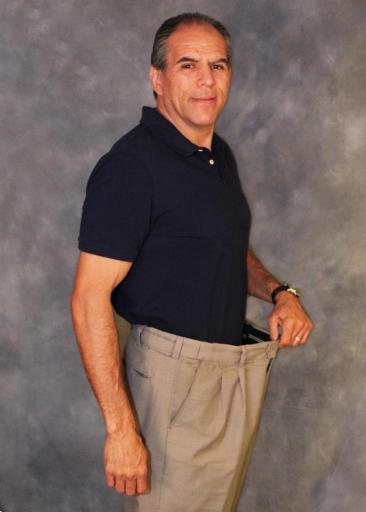
Success Story: Reversing Diabetes With a Plant-Based Diet
Growing up, Marc Ramirez thought that diabetes was inevitable. As a young adult, his mother and six of his siblings battled type 2 diabetes and suffered through side effects, including kidney and pancreas transplants, amputations, and dialysis. Eventually, Marc was diagnosed, too. He tried to improve his health by lowering his carb intake and exercising, but he soon found himself on daily insulin injections and four other medications. Frustrated and feeling hopeless, he asked his doctor if he would ever live a life without daily medications. When his doctor said, “no,” Marc decided to take his health into his own hands.
After hearing about the health benefits of a plant-based diet, he and his wife decided to give it a try. His new diet followed just a few simple rules: He would avoid animal products and keep it low in fat. Otherwise, he could eat as much as he wanted, without counting carbs or calories. Marc’s daily menu included foods like oatmeal with fruit, pasta primavera piled high with vegetables, and spicy black bean burritos. Under his doctor’s supervision, in less than two months, Marc was not only able to drop his daily insulin injections, but every last one of his medications. His glucose levels are now completely normal.
References
- Lara-Castro C, Garvey WT. Intracellular lipid accumulation in liver and muscle and the insulin resistance syndrome. Endocrinol Metab Clin North Am. 2008;37(4):841-856. doi:10.1016/j.ecl.2008.09.002
- von Frankenberg AD, Marina A, Song X, Callahan HS, Kratz M, Utzschneider KM. A high-fat, high-saturated fat diet decreases insulin sensitivity without changing intra-abdominal fat in weight-stable overweight and obese adults. Eur J Nutr. 2017;56(1):431-443. doi:10.1007/s00394-015-1108-6
- Srour B, Chazelas E, Druesne-Pecollo N, et al. Dietary exposure to nitrites and nitrates in association with type 2 diabetes risk: results from the NutriNet-Santé population-based cohort study. PLoS Med. 2023;20(1):e1004149. doi:10.1371/journal.pmed.1004149
- Fernandez-Cao JC, Arija V, Aranda N, et al. Heme iron intake and risk of new-onset diabetes in a Mediterranean population at high risk of cardiovascular disease: an observational cohort analysis. BMC Public Health. 2013;13:1042. doi:10.1186/1471-2458-13-1042
- Khalid M, Petroianu G, Adem A. Advanced glycation end products and diabetes mellitus: mechanisms and perspectives. Biomolecules. 2022;12(4):542. doi:10.3390/biom12040542
- O’Hearn M. Lara-Castor L, Cudhea F, et al. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat Med. 2023;29:982-995. doi:10.1038/s41591-023-02278-8
- Tonstad S, Butler T, Yan R, et al. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. 2009;32:791-796. doi:10.2337/dc08-1886
- Gu X, Drouin-Chartier JP, Sacks FM, Hu FB, Rosner B, Willett WC. Red meat intake and risk of type 2 diabetes in a prospective cohort study of United States females and males. Am J Clin Nutr. 2023;118(6):1153-1163. doi:10.1016/j.ajcnut.2023.08.021
- Zhang R, Fu J, Moore JB, Stoner L, Li R. Processed and unprocessed red meat consumption and risk for type 2 diabetes mellitus: an updated meta-analysis of cohort studies. Int J Environ Res Public Health. 2021;18(20):10788. doi:10.3390/ijerph182010788
- Vang A, Singh PN, Lee JW, Haddad EH, Brinegar CH. Meats, processed meats, obesity, weight gain and occurrence of diabetes among adults: findings from Adventist Health Studies. Ann Nutr Metab. 2008;52(2):96-104. doi:10.1159/000121365
- Sanders LM, Wilcox ML, Maki KC. Red meat consumption and risk factors for type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2023;77(2):156-165. doi:10.1038/s41430-022-01150-1
- Priebe MG, van Binsbergen JJ, de Vos R, Vonk RJ. Whole grain foods for the prevention of type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008;2008(1):CD006061. doi:10.1002/14651858.CD006061.pub2
- Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr. 2012;142(7):1304-1313. Doi:10.3945/jn.111.155325
- Barouti AA, Tynelius P, Lager A, Björklund A. Fruit and vegetable intake and risk of prediabetes and type 2 diabetes: results from a 20-year long prospective cohort study in Swedish men and women. Eur J Nutr. 2022;61(6):3175-3187. Doi:10.1007/s00394-022-02871-6
- Muraki I, Imamura F, Manson JE, et al. Fruit consumption and risk of type 2 diabetes: results from three prospective longitudinal cohort studies. BMJ. 2013;347:f5001. doi:10.1136/bmj.f5001
- Bondonno NP, Davey RJ, Murray K, et al. Associations between fruit intake and risk of diabetes in the AusDiab cohort. J Clin Endocrinol Metab. 2021;106(10):e4097-e4108. doi:10.1210/clinem/dgab335
- Ren Y, Sun S, Su Y, Ying C, Luo H. Effect of fruit on glucose control in diabetes mellitus: a meta-analysis of nineteen randomized controlled trials. Front Endocrinol (Lausanne). 2023;14:1174545. doi:10.3389/fendo.2023
- Yoon E, Bae JC, Suh S. Intake of fruit and glycemic control in Korean patients with diabetes mellitus using the Korea National Health and Nutrition Examination Survey. Endocrinol Metab (Seoul). 2023;38(5):538-544. doi:10.3803/EnM.2023.1730
- Meng Y, Li S, Khan J, et al. Sugar- and artificially sweetened beverages consumption linked to type 2 diabetes, cardiovascular diseases, and all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutrients. 2021;13(8):2636. doi:10.3390/nu13082636
- Tseng TS, Lin WT, Gonzalez GV, Kao YH, Chen LS, Lin HY. Sugar intake from sweetened beverages and diabetes: a narrative review. World J Diabetes. 2021;12(9):1530-1538. doi:10.4239/wjd.v12.i9.1530
- Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777-1783. doi:10.2337/dc06-0606
- Kahleova H, Tura A, Hill M, Holubkov R, Barnard ND. A plant-based dietary intervention improves beta-cell function and insulin resistance in overweight adults: a 16-week randomized clinical trial. Nutrients. 2018;10(2):189. doi:10.3390/nu10020189
- Kahleova H, Petersen KF, Shulman GI, et al. Effect of a low-fat vegan diet on body weight, insulin sensitivity, postprandial metabolism, and intramyocellular and hepatocellular lipid levels in overweight adults: a randomized clinical trial. JAMA Netw Open. 2020;3(11):e2025454. doi:10.1001/jamanetworkopen.2020.25454
- Campbell TM, Campbell EK, Attia J, et al. The acute effects of a DASH diet and whole food, plant-based diet on insulin requirements and related cardiometabolic markers in individuals with insulin-treated type 2 diabetes. Diabetes Res Clin Pract. 2023;202:110814. doi:10.1016/j.diabres.2023.110814
- Gummesson A, Nyman E, Knutsson M, Karpefors M. Effect of weight reduction on glycated haemoglobin in weight loss trials in patients with type 2 diabetes. Diabetes Obes Metab. 2017;19(9):1295-1305. doi:10.1111/dom.12971
- Reynolds AN, Akerman AP, Mann J. Dietary fibre and whole grains in diabetes management: systematic review and meta-analyses. PLoS Med. 2020;17(3):e1003053. doi:10.1371/journal.pmed.1003053